
Spinal stenosis Treatment
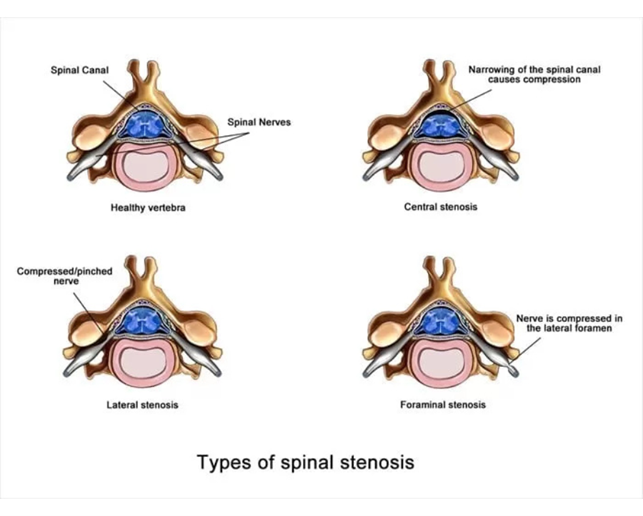
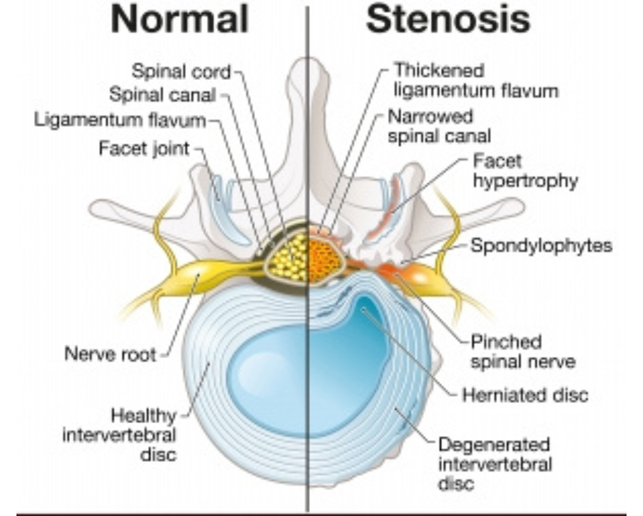
There are two important neural structures in the lumbar spine, dural sac and nerve root. The dural sac is a bag containing several nerve roots and lies in the center of spinal canal. A pair of nerve roots leave the dural sac at each level of lumbar spine and pass through lateral recess, foramen and extraforaminal area. The space should be adequate for the dural sac and nerve root to pass through, which if compromised start causing neurologic symptoms to the patient. This narrowing of the space for dural sac or nerve root is called spinal stenosis. The area stenosed determines the name of the stenosis like central canal stenosis, lateral recess stenosis or foramina stenosis. Central canal stenosis compresses the dural sac whereas lateral recess and foramina stenosis compresses the nerve root.
What causes spinal stenosis?
The structure of spine mainly responsible for spinal stenosis are ligamentum flavum and enlarged bone of facet joint and lamina. Spine stenosis occurs due to age related wear and tear of the spine. Ligamentum flavum gets calcified and facet joint gets arthritic. Therefore stenosis is a disease of elderly population around 55-60 years of age. Lifestyle factors like prolonged sitting or travelling, obesity, improper posture, sedentary lifestyle etc. can accelerate the wear and tear causing spinal stenosis to manifest at a younger age, say in 30’s and 40’s.
What are symptoms of spinal stenosis?
Symptoms depend on the part of spinal canal getting stenosed.
Central canal stenosis obviously causes dural sac to get compressed. Dural sac compression produces following features:
- Burning sensation or heaviness generally in both legs and rarely in one leg while walking
- Neurogenic claudication, meaning inability to walk for long distance in one stretch. These patients usually develop burning sensation while walking due to which they have to take frequent rests. The distance they walk in a single go is called claudication distance and is usually few meters (200-500m)
- Pain relieved on bending forward, going uphill or climbing upstairs
- Loss of bowel and bladder control in severe stenosis
- Lateral recess presses on the traversing nerve root and produce sciatica like symptoms which are:
Radiating pain from low back to thigh, leg and foot
- Numbness, tingling or heaviness of thigh, leg and foot
- Weakness of ankle or toes. These are commonly perceived as inability to lift the foot off the ground while walking (foot drop) or inability to straighten the toes (toe drop)
- Foraminal stenosis presses on the exiting nerve root. Symptoms are sciatica like symptoms like that of lateral recess stenosis but area of symptoms in leg and foot correspond to the exiting nerve root.
When is surgery required for spinal stenosis?
Surgery for spine stenosis is advised if all the conservative methods of treatment (such as medications, physical therapy and spine injections) have failed to provide relief. Main indications for surgical decompression of stenosis are:
- Severe pain: Persistent or worsening leg or back pain not responding to conservative treatments
- Difficulty walking: Claudication (pain or burning sensation in legs) that limit daily activities or ability to walk even short distances
- Neurological symptoms: Progressive weakness in ankle or toes, progressive numbness or tingling in legs indicating significant nerve root compression
- Bowel and bladder incontinence: Also called caudal equine syndrome, is a surgical emergency and should be operated as early as possible
Surgical options for spinal stenosis
The problem causing structure in spinal stenosis that compress the thecae sac or nerve roots are mainly hypertrophied ligamentum flavum and enlarged bone (of facet joint or lamina). An ideal surgery for spinal stenosis should:
- Decompress the neurological structure by removing the offending tissue
- Preserve the normal anatomic tissues as much as possible (Minimum collateral tissue damage)
Surgeries for spinal stenosis include endoscopic decompression, microscopic decompression and open decompression. All of these can effectively remove the hypertrophied ligamentum flavum and bone but how much destruction is caused to the normal tissue is the deciding factor for long term success of surgery.
- Endoscopic decompression: In endoscopic decompression, the ligamentum flavum and facet is targeted directly without damaging the surrounding tissues with help of specialized camera system called endoscopes. It is least invasive form of decompression. There is minimum incision, few or no stitches, minimum blood loss, early rehabilitation and quick recovery. Collateral tissue damage is minimum amongst all the techniques of decompression and therefore long term pain relief is best.

- Microscopic decompression: The offending structure is targeted with help of tubular retractors and microscope. This is also a less invasive form of surgery but collateral tissue damage is more than endoscopic technique.

- Open decompression: This is the conventional and original form of surgery. Here all the structures superficial to the problem causing structure are damaged to gain access and there is more of collateral tissue damage. These tissues include the muscles, supraspinous and interspinous ligaments, lamina etc that are important to spine stability. Also, open surgery involves bigger incision, more blood loss, prolonged rehabilitation and longer recovery time.

What endoscopic surgery do we do for spine stenosis?
- We do uniportal spine endoscopy for stenosis treatments, both by transforaminal and interlaminar technique.
- This is the best form of stenosis treatment available worldwide at present. The type of surgery depends on the location of the prolapsed disc.
- We evaluate the patient first clinically and then radiologically with MRI and ascertain the position of disc.
Central stenosis: Central stenosis may cause compression of central parts of thecal sac. It can be addressed by resection of the impinging bone of facet and hypertrophied ligamentum flavum using an ipsilateral full endoscopic interlaminar approach with additional extension of the procedure to the contralateral side (over the top technique)
Lateral recess stenosis: It causes compression of the traversing nerve root and lateral portions of thecal sac. This is best addressed by careful reaction of bone and ligamentum flavum through a full endoscopic interlaminar approach. A variety of burrs and Kerrison rongeurs are used to remove the impinging bone and soft tissue.

Search Keywords:
spinal stenosis, lumbar spinal stenosis, spinal stenosis treatment, cervical spinal stenosis, spinal stenosis symptoms, stenosis,spinal stenosis pain, what is spinal stenosis, lumbar stenosis, lumbar spinal stenosis treatment, what causes cervical spinal stenosis, spinal stenosis best treatment, best spinal stenosis treatment in india, best spinal stenosis treatment in delhi, best spinal stenosis treatment in gurugram, best spinal stenosis treatment in ncr, best spinal stenosis treatment in uttar pradesh, best spinal stenosis treatment in agra, best spinal stenosis treatment in by dr dhruv sharma, best spinal stenosis treatment in faridabad,


