
Endoscopic Spine Surgery
Endoscopy of spine (Save the Spine)Spine endoscopy is the most refined form of spine surgery. It has eliminated the need for an elaborate or traditional open spine surgery for pinpoint pathologies in spine. The disease of spine where the target unhealthy structure lies deep in the spine but its removal needs the invasion of several healthy structures to gain access, now can be removed precisely with help of camera and leaving the healthy structures intact. For this reason endoscopy is obviously the most revolutionary technique of spine surgery.
Basic Concept of endoscopic spine surgery
There is a saying “To throw the baby out with the bathwater” that conveys the idea of loosing something valuable while trying to get rid of something undesirable. This is exactly what happens in open spine surgery. A lot of normally functioning tissues get damaged in open spine surgery. This damage is called ‘collateral tissue damage.’ The damage once made is irreversible and makes spine incapable of withstanding the injuries of day to day activities causing secondary degeneration and long term pain. Endoscopic spine surgery is a revolutionary technology of performing a spine decompression (removing the offending tissue) by bypassing all the innocent but important structures by targeting the offending tissue directly using specialised instruments. Hence there is no collateral tissue damage and spine is left virgin as before even after the surgery is done. There is no secondary instability and long term pain control is wonderful.
Why is collateral tissue damage indispensable in open spine surgeries?
Spine is a very deep structure in body. Whenever a person suffers from sciatica, slipped disc or spinal stenosis, we target to remove the problem causing structure of to relieve the patient of his symptoms. This offending structure may be a disc or osteophyte or bony spur or ligamentum flavum. These offending structures lie deep in the spine. Open spine surgery requires removal of multiple normally functioning tissues that lie between the skin and these offending structures.
What are these collateral tissues, what are their roles in brief and what effect the open spine surgery have on them?
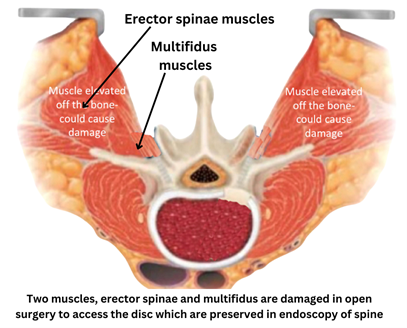
Muscles: Variable degree of damage occurs to two important muscles, erector spinae and multifidus muscle. Erector spinae is a ‘movement muscle’ that enable us to stand erect. Damage to this muscle causes stooped posture, slouching and secondary degeneration of spine and pain. Multifdus is a ‘stability muscle’. It keeps you vertebrae stable when the spine is moving, like when we lift a weight or perform any activity that involves back movement. Damage to multifidus muscle allows unsynchronised movements to occur causing secondary degeneration of spine and long term pain.
Ligaments:
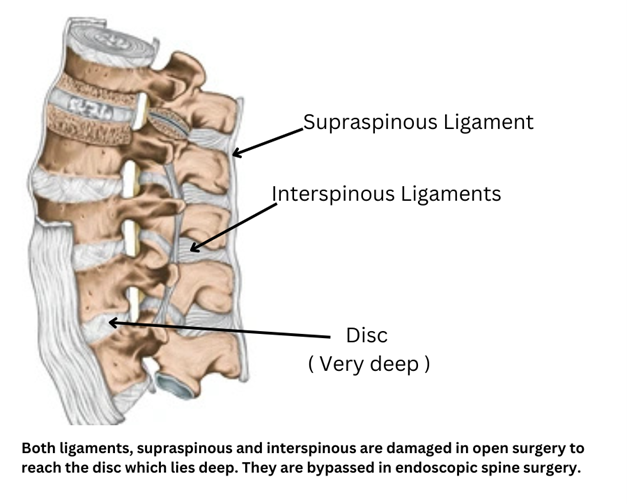
Ligaments are tight structures that don’t allow movement beyond physiological range between two bones.Two ligaments, supraspinous ligaments and interspinous ligaments get damaged in open spine surgery tampering the stability of spine.
Bone:
Spinous process and lamina, part of spine crucial to stability of spine is removed to gain access to the disc compromising spine stability.
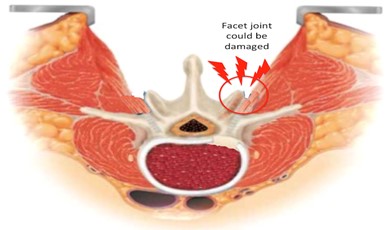
Joint: Facet joint, an important structure for maintaining both mobility and stability of spine may get damaged destabalising the spine grossly.
Ligamentum flavum:
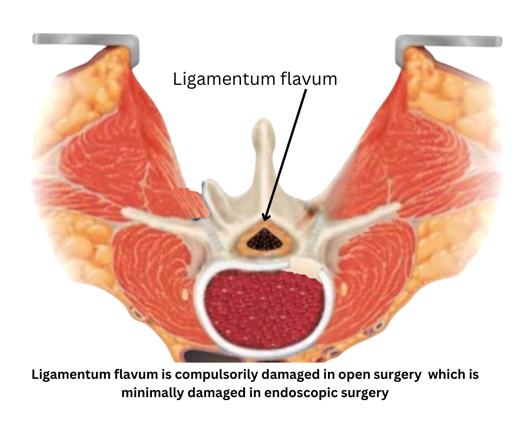
Ligamentum flavum acts a very important barrier between the nervous structures and muscles. Its damage causes adhesions between these two structures and neurogenic pain secondry to these adhesions. All open surgeries damage this ligament but with endoscopy we can bypass this ligament or limit its damage to the minimum.
What are the benefits of spine endoscopy?
By virtue of spine endoscopy being the most minimally invasive form of spine surgery and causing minimum collateral damage, it offers the following benefits:
- Long term and sustained pain relief
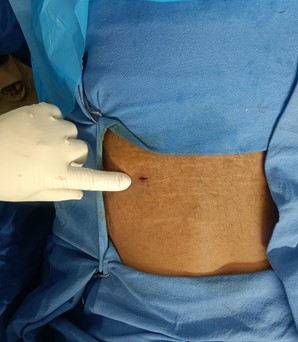
- Stitchless surgery or minimal stitches
- Minimal blood loss
- New day ambulation
- Same or next day discharge
- Early rehabilitation
- Faster return to work
- No need of general anaesthesia in specific cases

What spine conditions can be treated with spine endoscopy?
- Slipped disc : Slipped disc or prolapsed intervertebral disc commonly known as sciatica is a condition where a part of disc slips out of its normal position compressing the neural structues. The patient complains of pain from the low back to the back of thigh and leg upto foot. Beauty of spine endoscopy in slipped disc management is endoscope has a good mobility and can be moved around to hunt for the problematic disc fragment, even in difficult locations (extraforaminal discs, migrated discs etc.) while causing minimum collateral damage.
- Spinal stenosis : Here the patient has sciatica like symptoms along with difficulty in walking, heaviness or burning sensation in legs while walking. Problem causing structures are discs, ligamentum flavum or osteophytes. There structures again lie deep in the spine and can be targeted with endoscopy without causing unnecessary collateral damage.
- Spondylolisthesis : This is a condition where two vertebrae are not stable on each other and move abnormally causing severe backpain with or without sciatica. Target of surgery is to fuse the spine by removing whole of the disc and put screws in the two vertebra to eliminate abnormal movements. Traditionally this condition was dealt with open surgery, surgery called as TLIF (Transforaminal lumbar inter body fusion). It had a lot of collateral tissue damage, lot of blood loss and longer recovery time. With advancements in endoscopy, TLIF is done with endoscopic technique and called endofusion.
- Facet pathologies: Facetal cysts or hypertrophied facet joints may press on the neural structures causing sciatica or spine stenosis. Specifically targeting these facet joints with endoscopes eliminate the need to damage the collateral tissues increasing the success rates of these surgeries.
- Spine infections: Infections of spine commonly start with the disc, a condition called as discitis. Disc can be derided and pus can be drained well with endoscopes, an example of a minimally invasive approach for a deep seated problem.
- Spine tumors: In selective cases, benign spine tumors can be targeted with spine endoscopy to eliminate need of a more aggressive open surgery.
What we don’t do in name of spine endoscopy?
By now it is clear that endoscopy stands true to its name only if it sacrifices minimal health tissue, not only on the outside (skin), but also on the inside (collateral tissue). I say this because there are multiple variations of spine endoscopy in the market that may cause very little damage on the skin but a lot to the collateral tissues that lie deep to skin. We do the ideal form of spine endoscopy called ‘uniportal spine endoscopy.’ Of all the variations, this is the true form of spine endoscopy. The variations to this type (that we of course don’t do)
are:
- Tubular technique: This is also a minimally invasive technique of spine surgery but it is not endoscopy. It uses tubular retractors and microscopes. The incision is at least an inch compared to 8-10mm used in uni portal technique. Also the collateral tissue damage is much higher than in uni portal endoscopy.
- Unilateral biportal endoscopy (UBE): Though the skin incisions are small but a lot of collateral tissue damage is happening inside the skin which is not visible outside. It doesn’t stand true to the name of true spine endoscopy.
- Destandau’s technique: It causes further more damage to collateral tissue than UBE technique.
What are the techniques of uniportal spine endoscopy?
There are two standard techniques of spine endoscopy, transforaminal technique and inter-laminar technique. Both of these are techniques are of uniportal spine endoscopy. Any of these two techniques can be used depending on location of diseased structure and extend of decompression required.
- Transforaminal spine endoscopy

- Transforaminal endoscopy is so named because here we access the spine through the natural orifice in the spine called the ‘intervertebral foramen.’
- It used to target unilateral foraminal or extraforaminal or lateral recess disc prolapse or isolated stenosis of these regions.
- This surgery is done under local anaesthesia, that means the patient is totally awake during the surgery and can talk to the doctor during the procedure in case any discomfort is felt.
- Therefore this technique is good for morbid patients who are not fit for general anaesthesia.
- Interlaminal spine endoscopy:
- Interlaminar spine endoscopy is so named because here the spine is accessed through another natural orifice in spine called the ‘inter laminar window.’
- It is used for ligamentum flavum pathologies of central canal or lateral recess, central disc pathology or bilateral extraforaminal, foraminal or lateral recess pathology.
- The surgery is done under general anaesthesia.


